THE CMS GUIDE MODEL
Earlier this year, CMS introduced the GUIDE model, short for “Guiding an Improved Dementia Experience.” This optional program is designed to enhance the well-being of individuals with dementia and their informal/family caregivers by emphasizing care coordination and support for caregivers in the delivery of care.
This groundbreaking program represents a shift in acknowledging the significant impact that informal/family caregivers can have on the health and medical outcomes of patients under their care.
Unlike previous CMS programs focused on cost reduction, the GUIDE program is unique in its goal to prioritize and fund caregiver support without aiming for shared savings or cost reduction evaluations. The program recognizes the vital role of family caregivers in influencing health outcomes and aims to provide enhanced support to alleviate the challenges of caring for patients with Alzheimer’s, ultimately leading to better patient care.
By addressing the needs of family caregivers, the program seeks to improve both the physical and emotional well-being of caregivers, resulting in better health outcomes. Research shows that patients with caregivers who are struggling emotionally or physically tend to have higher medical costs and increased emergency department visits. In contrast, involving family caregivers in care plans has been linked to a significant decrease in hospital readmissions, highlighting the crucial role of caregiver support in enhancing overall patient health outcomes.
Understanding The CMS’s GUIDE Program
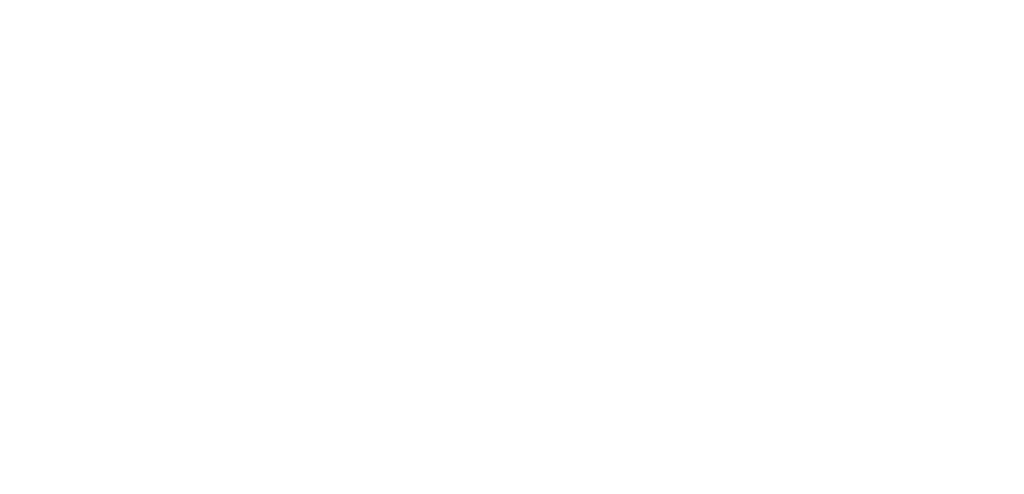
Now that we have established the rationale behind our efforts, let’s delve into the specifics of what GUIDE will do to enhance caregiver support. The program aims to enhance quality of life, alleviate caregiver burden, and enable individuals with dementia to remain in their homes for longer periods by focusing on the following key components:
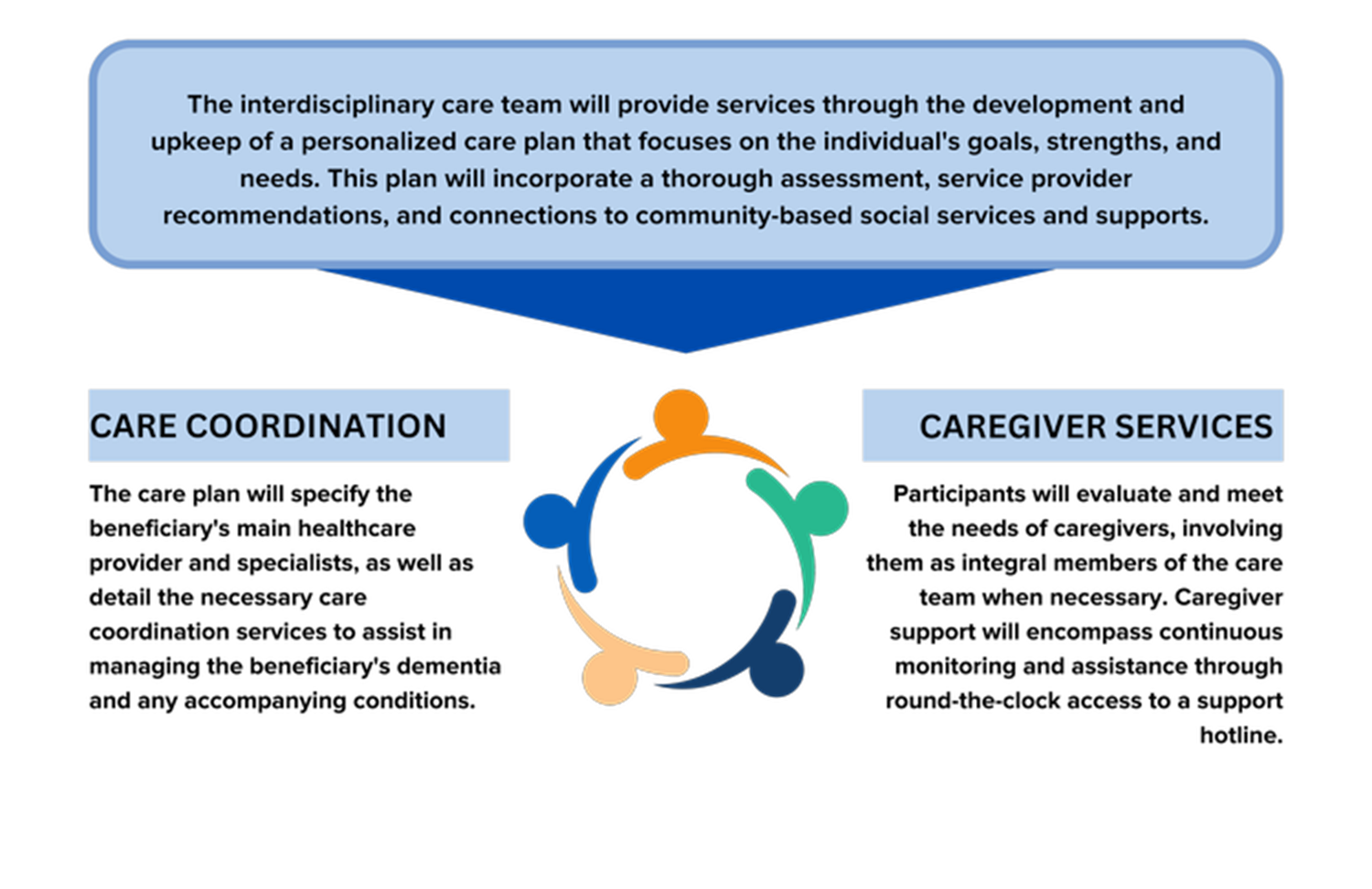
1. Care Coordination & Management: Patients will benefit from an interdisciplinary team that will develop a personalized care plan, assess the progression of their condition, and provide ongoing monitoring and care.
2. Caregiver Support & Education: Participants will receive caregiver support through training, educational resources, and support groups. Additionally, a dedicated Care Navigator will be available to assist caregivers in accessing the necessary services and support, both clinical and non-clinical.
3. Respite Services: Eligible caregivers will have access to free respite services, with a value of up to $2,500 per year.
The most novel pillar in this program’s structure is caregiver support. Each participant must ensure they have the content, expertise, and resources in place before enrolling in the program, something that has not been traditionally required in most clinical settings. These requirements are comprehensive:
- Navigation: A dedicated expert is there to help facilitate communication, appointments, medication needs with the clinical care team, and referrals to community-based services including meal and transportation assistance.
- 24/7 support line: Beneficiaries and caregivers must have access to a member of their care team or Care Navigator using a 24/7 helpline
- Training: On-demand access to comprehensive educational classes, content, and support groups on a wide array of topics related to dementia caregiving.
- Medication management: The clinical team regularly reviews prescribed medication as needed, while care navigators provide tips for patient and caregiver to successfully adhere to medication regimens.
The Mechanics Of The GUIDE Model
The final aspect of comprehending the GUIDE model involves understanding the operational details. This includes how the model will be implemented, how patients will qualify for participation, and how both CMS and participants can assess the impact and effectiveness of the model.
The program will officially began in July 2024 and will last eight years. Eligible patients must:
- Have a dementia diagnosis
- Have Medicare as their payer
- Be enrolled in Medicare Parts A & B (not Medicare Advantage or PACE)
- Not be enrolled in Medicare hospice benefit
- Not be residing in a long-term nursing home (assisted living facilities are accepted)
Periodic assessments will be conducted throughout the program. This presents a new opportunity for many current value-based providers to leverage the resources offered by the GUIDE model in order to lower care costs.
Participants are required to collect and report data and will be evaluated based on:
- Care Coordination and Management: High-risk medications (eCQM/CQM)
- Patient quality of life: Quality of life outcome (Survey-based)
- Caregiver Support/Burden: Zarit Burden Interview (Survey-based)
- Utilization: Total Per Capita Cost (Claims-based)
- Long-term nursing home stay rate (Claims-based)
In Conclusion
The GUIDE model marks a new chapter in the way our culture acknowledges and addresses all of the non-clinical care deeply impacting clinical outcomes. For too long, the pivotal work of family caregivers has been hidden and taken for granted by our healthcare and social systems. This model serves as a first step toward placing tangible value on that work.
By integrating them into the care team and supporting their participation, we can improve the holistic care experience for patients, improving their quality of life and keeping them at home longer.
Contact a GUIDE Ambassador Today!
Phone: (321)235-0692 | Fax: (321) 234-0694 | Email: [email protected]